Understanding Canine Cushing's Syndrome
Knowledge of the pathophysiology of Cushing’s Syndrome helps you to understand what changes to expect in your patient presenting with Cushing’s.
In this section, we will re-cap the causes and clinical signs of Cushing’s syndrome to help you recognise your next case.
What is Canine Cushing's syndrome?
Cushing's syndrome is the term used to describe a combination of clinical and biochemical abnormalities resulting from chronic exposure to excessive amounts of glucocorticoids.
Hypercortisolism is the term used for excessive glucocorticoid activity due to cortisol.
What are the different types of Cushing's syndrome?
Cushing's can either be naturally occurring (spontaneous) or iatrogenic.
- In naturally occurring Cushing's, there is chronic overproduction of glucocorticoids (predominantly cortisol) by the adrenal glands.
- Iatrogenic Cushing's results from chronic administration of exogenous glucocorticoids.
How is cortisol produced?
Cortisol is produced in the zona fasciculata and zona reticularis of the adrenal cortex. In the normal dog, cortisol release is stimulated by adrenocorticotrophic hormone (ACTH), which is released from the anterior pituitary gland. The release of ACTH is regulated by a corticotropin releasing hormone (CRH) secreted from the hypothalamus.
Cortisol also has a negative feedback effect on the anterior pituitary gland to decrease production of ACTH and ensure that plasma cortisol levels remain in balance.
Naturally occurring Cushing's syndrome
Specialists recommend categorising naturally occurring Cushing’s syndrome in to two classes. These are based on whether the cause is dependent or independent of ACTH production (ESVE, 2021).
Within these two classes we recognise the most common causes:
addACTH - Dependent Cushing's syndrome
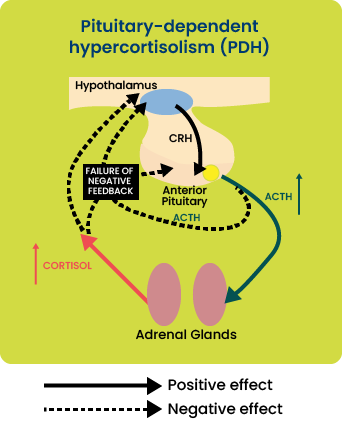
Pituitary-dependent hypercortisolism (PDH):
Most cases of naturally occurring Cushing’s syndrome (80-85%) are caused by hypersecretion of ACTH by a lesion in the pituitary gland, typically pituitary neoplasia or hyperplasia.
This leads to bilateral adrenal hyperplasia and increased glucocorticoid concentration in the blood (hypercortisolism).
Dogs with PDH have a failure of the normal negative feedback mechanism which should prevent excess circulating cortisol. This is demonstrated in Figure 1.
Rarer forms of ACTH-dependent hypercortisolism:
- Ectopic ACTH, where excessive ACTH is produced from a site away from the pituitary gland.
- Sub diagnostic Cushing’s syndrome, where clinical symptoms of Cushing’s syndrome are displayed, and excessive ACTH secretion is demonstrated, yet subsequent increases in cortisol cannot be proven.
addACTH - Independent Cushing's syndrome
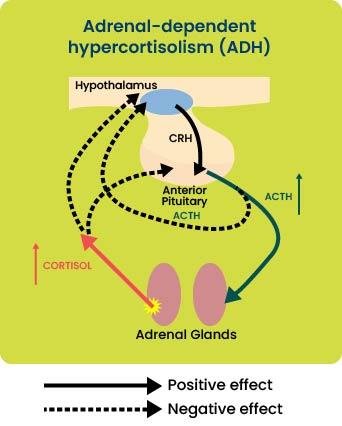
Adrenal-dependent hypercortisolism (ADH):
15-20% of cases of naturally occurring Cushing’s syndrome are due to unregulated cortisol secretion by the adrenal cortex, generally associated with adrenal neoplasia, resulting in hypercortisolism.
The increased serum cortisol concentration results in suppression of pituitary ACTH secretion and subsequent
atrophy of non-tumorous adrenocortical tissue. This is demonstrated in Figure 2.
Rarer forms of ACTH-independent hypercortisolism:
- Aberrant adrenal receptor expression, including food-dependent hypercortisolism.
- Sub diagnostic Cushing’s syndrome, where clinical symptoms of Cushing’s syndrome are displayed due to secretion by an adrenal tumour of a non-cortisol hormone that has glucocorticoid activity.
addIs there a typical signalment?
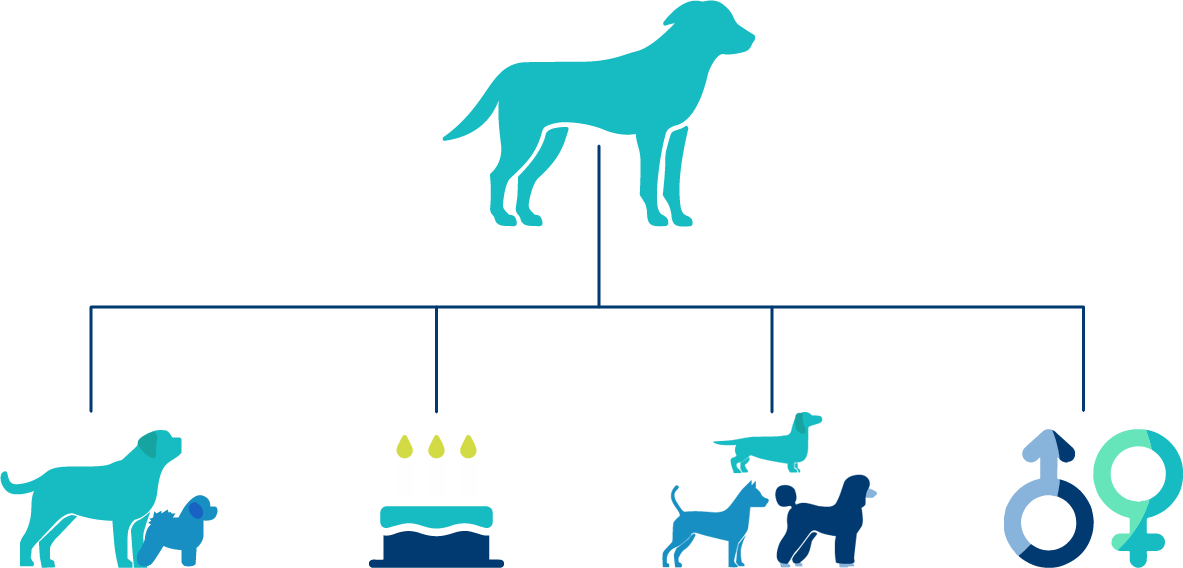
Dogs with Cushing's come in many shapes and sizes.
Think back to cases of Cushing's that you have previously dealt with or read about: are there any breeds that seem to be more commonly affected? What is the mean age at diagnosis? Is Cushing's more common in male or female dogs?
Top Tip
Larger dogs tend to display a single, often more pronounced clinical sign of Cushing's, whereas smaller dogs may display many clinical signs.
Age
PDH is usually diagnosed in middle-aged to older dogs (median age 7-9 years), whereas ADH is seen most commonly in older dogs (median age 11-12 years).
Breeds
Cushing's can occur in many breeds, but Poodles, Dachshunds and small terriers appear to be at greater risk of developing PDH. ADH occurs more frequently, though not exclusively, in larger breeds of dog.
Sex
There is no significant difference in sex distribution for PDH. However, female dogs are more likely to develop ADH.
What are the clinical signs of Cushing's syndrome in dogs?
The clinical signs of Cushing’s syndrome can be categorised by how frequently they are identified at the time of initial presentation of the patient to the clinic (Behrend et al, 2013).
addSymptoms seen commonly
Symptoms seen commonly
- Polydipsia (increased thirst)
- Polyuria (increased frequency of urination)
- Polyphagia (increased appetite)
- Panting
- Abdominal distention (otherwise known as a ‘pot belly’ and sometimes confused with weight gain or fluid retention)
- Alopecia (hair loss - mainly seen on the flanks and extremities.) Note that atopic dermatitis /pruritic conditions are NOT commonly associated with such an alopecia. The elevated production of glucocorticoids from the adrenal cortex as part of this disorder ‘mask’ any itch
- Hepatomegaly (enlargement of the liver)
- Muscle weakness
- Systemic hypertension (increased blood pressure)
The image to the left shows a typical ‘rat tail’ which can be seen with alopecia of endocrine origin.

addSymptoms seen less commonly
Symptoms seen less commonly
- Lethargy (or fatigue)
- Hyperpigmentation
- Comedones (‘black heads’)
- Thin skin
- Poor hair regrowth (after clipping for a blood sample or a groom for example)
- Urine leakage
- Insulin resistant diabetes mellitus
The image to the left shows lack of hair regrowth some time after blood sampling.

addSymptoms seen rarely
Symptoms seen rarely
- Thromboembolism (blood clot)
- Ligament rupture
- Facial nerve palsy
- Pseudomyotonia
- Testicular atrophy (entire male dogs)
- Persistent anaestrus (entire female dogs)
The image to the left shows a dog with pseudomyotonia.

© Carlos Melian
