Haematologically, a lack of a stress leukogram in an unwell patient, and in particular the presence of a lymphocytosis or eosinophilia, should move hAC up the list of differentials. It is worth noting that results may still be within normal reference range and this highlights the importance of looking at all parameters – even if deemed to be ‘normal’. PCV can be variable in dogs with hypoadrenocorticism, some may show a non-regenerative anaemia but this may be masked due to the presence of dehydration (Scott-Moncrieff, 2015).
Diagnosing Dogs with Hypoadrenocorticism
How is hypoadrenocorticism diagnosed?
Routine haematology, biochemistry and urinalysis are recommended as the starting point for diagnosis of most endocrine conditions. This will rule out other causes of illness and often shows non-specific changes which will increase the index of suspicion.
Haematology add
Biochemistry add
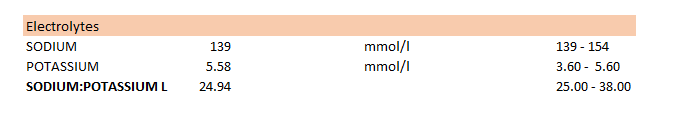
The main biochemical abnormalities seen are electrolyte disturbances. The vast majority of cases will have a decreased sodium to potassium ratio (<27) due to a hyperkalaemia and a hyponatraemia (Peterson et al, 1996). However, there are other disease processes which can lower this ratio – making it a non-specific finding. Equally, many routine biochemical blood profiles do not include electrolytes as standard, and where they do, the Na:K ratio is not automatically generated. Therefore, a biochemical report may appear normal even if the patient truly has hAC.
An example is shown in the table below. The absolute values for sodium and potassium sit within the reference range for this patient, therefore are not highlighted as abnormal on the biochemistry report. However, when the ratio is calculated it reveals a low value and therefore hypoadrenocorticism should still be included as a differential.
Other changes in biochemistry which may be seen include azotaemia, decreases in albumin, glucose, cholesterol and chloride levels, alongside increases in ‘liver’ enzymes (ALKP, ALT and AST), phosphate and calcium (Peterson et al, 1996).
Urinalysis add
Typically, dogs with hypoadrenocorticism have a urine specific gravity (USG) of <1.030. This can complicate matters even further for the clinician. The presence of azotaemia, increased phosphate and low USG in an ill patient may point towards acute renal failure. This highlights the requirement for specific endocrine testing in these cases, without which it may be difficult to decide upon a definite diagnosis.
Endocrine testing add
The combination of history, clinical signs and routine laboratory findings will often lead to increased suspicion of hypoadrenocorticism. However, specific endocrine testing is then required to confirm diagnosis.
1. What is the best test to use to diagnose hypoadrenocorticism?
The ACTH stimulation test (ACTHST) is the gold standard test for diagnosing hypoadrenocorticism in dogs.
2. How do I interpret an ACTHST?
A deficiency in post-ACTH cortisol indicates the presence of hypoadrenocorticism. This usually equates to a value of < 55 nmol/L (< 2 μg/dL) as depicted in Graph One. However, it is recommended that you consult your specific laboratory for reference ranges specific to your results.
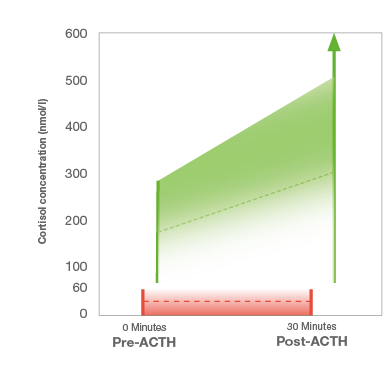
- Graph One – Interpretation of the ACTH stimulation test
- Key
- Green – Not hypoadrenocorticism
- Red – Hypoadrenocorticism or steroid administration
3. When might I get a false positive result for hypoadrenocorticism using the ACTHST?
Unfortunately, the administration of exogenous glucocorticoids before undertaking an ACTHST can lead to false positive results. It is therefore essential to gain a thorough history when undertaking a work-up for a suspected case of hAC, given that even small exposure to glucocorticoids can lead to suppression of the hypothalamic-pituitary adrenal axis which could be interpreted as a positive result for hAC.
Exogenous glucocorticoids are not limited to oral or injectable preparations, consideration should also be given to topical therapies (most often for the skin, ear or eye) and owner administered preparations.
A summary of the diagnosis of hypoadrenocorticism can be downloaded below
Eunatraemic, eukalaemic hypoadrenocorticism
The European Society of Veterinary Endocrinology ALIVE committee, define eunatraemic, eukalaemic hypoadrenocorticism as hAC with normal serum concentrations of potassium and sodium (European Society of Veterinary Endocrinology ALIVE Committee, 2021). Previously this type of hAC has been referred to as ‘atypical Addison’s disease’.
These dogs present with the same, often chronic, clinical signs of primary hAC, but do not have the characteristic changes in electrolytes. Other non-specific biochemical findings, such as hypocholesterolaemia and hypalbuminaemia may point towards disease, but diagnosis is challenging.
How is eunatraemic, eukalaemic hypoadrenocorticism diagnosed? add
It is recommended to measure both aldosterone and endogenous ACTH in these cases in order to truly define the condition and therefore such cases may benefit from the advice of an internal medicine specialist.
Measurement of endogenous ACTH
As stated in the section ‘What is hypoadrenocorticism?’, there are two main types of hypoadrenocorticism. Clinical signs can arise due to a deficiency in the adrenal gland itself (primary disease) or due to a deficiency of stimulation by the pituitary (secondary disease). It is possible to differentiate between primary and secondary disease by the measurement of endogenous ACTH (eACTH).
In primary disease, (including eunatraemic, eukalaemic hypoadrenocorticism), eACTH should be elevated, as the pituitary detects the low circulating levels of cortisol and releases ACTH to compensate.
In secondary disease, eACTH will be low, as it is a failure of ACTH production which is the cause of disease. Secondary disease should be ruled out before confirming eunatraemic, eukalaemic hypoadrenocorticism.
Aldosterone measurement
By measuring cortisol after stimulation by ACTH, there is an assumption that this reflects all hormone production by the adrenal gland. However, isolated hormone deficiencies can occur. The only true way of knowing if a dog is able to produce mineralocorticoid is by measuring aldosterone itself. This is done in the same way as the ACTHST, and can allow you to determine if aldosterone supplementation is truly required as part of the treatment plan.

